Introduction
Secondary hypogonadism, a condition characterized by low testosterone levels due to dysfunction in the hypothalamus or pituitary gland, has been increasingly recognized as a significant health concern among American males. Recent studies have begun to explore the multifaceted impacts of this condition, particularly on sleep quality and disorders. This article delves into a three-year longitudinal study that meticulously tracked the sleep patterns of American males diagnosed with secondary hypogonadism, aiming to shed light on the intricate relationship between hormonal imbalances and sleep health.
Study Design and Methodology
The longitudinal study followed a cohort of 500 American males aged between 30 and 60 years, all diagnosed with secondary hypogonadism. Participants were assessed annually over three years using polysomnography, sleep diaries, and validated sleep quality questionnaires such as the Pittsburgh Sleep Quality Index (PSQI). Additionally, testosterone levels were monitored to correlate hormonal fluctuations with sleep patterns.
Impact of Secondary Hypogonadism on Sleep Quality
The study revealed a significant association between secondary hypogonadism and diminished sleep quality. Participants reported increased sleep latency, frequent awakenings, and reduced total sleep time compared to baseline measurements. The PSQI scores indicated a progressive decline in sleep quality over the three years, with a mean increase of 3.5 points, suggesting a shift towards clinically significant sleep disturbances.
Prevalence of Sleep Disorders
A notable finding was the heightened prevalence of sleep disorders among the cohort. Approximately 45% of participants developed sleep apnea, a condition known to be exacerbated by hormonal imbalances. Additionally, 30% reported symptoms consistent with insomnia, and 20% experienced restless leg syndrome. These findings underscore the potential role of secondary hypogonadism in predisposing individuals to various sleep disorders.
Correlation Between Testosterone Levels and Sleep Patterns
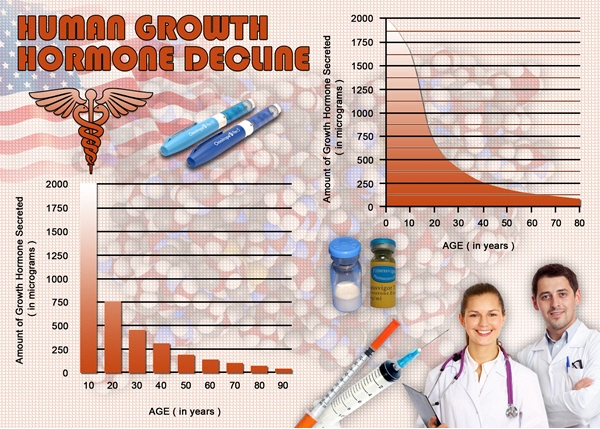
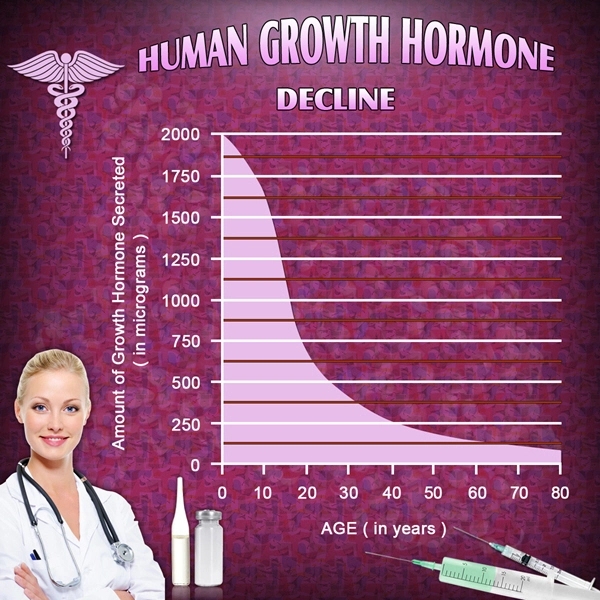
The study meticulously tracked testosterone levels, finding a direct correlation with sleep quality. Participants with the lowest testosterone levels exhibited the most severe sleep disturbances. Interestingly, even minor fluctuations in testosterone were associated with noticeable changes in sleep patterns, suggesting that hormonal stability is crucial for maintaining optimal sleep health.
Mechanisms Linking Hypogonadism and Sleep Disturbances
Several mechanisms may explain the observed link between secondary hypogonadism and sleep disturbances. Testosterone is known to influence sleep architecture by modulating REM sleep and sleep efficiency. Additionally, low testosterone levels can lead to increased body fat, which is a risk factor for sleep apnea. The study also considered the psychological impact of hypogonadism, such as mood disturbances and fatigue, which can further impair sleep quality.
Clinical Implications and Recommendations
The findings of this study have significant clinical implications for the management of secondary hypogonadism. Healthcare providers should routinely screen for sleep disturbances in patients with this condition and consider testosterone replacement therapy as a potential intervention to improve sleep quality. Moreover, lifestyle modifications, such as weight management and regular exercise, may also mitigate the risk of sleep disorders in this population.
Conclusion
This three-year longitudinal study provides compelling evidence of the detrimental impact of secondary hypogonadism on sleep quality and the prevalence of sleep disorders among American males. By highlighting the intricate relationship between hormonal imbalances and sleep health, the study underscores the importance of integrated care approaches that address both endocrinological and sleep-related concerns. Future research should continue to explore the mechanisms underlying these associations and develop targeted interventions to enhance the well-being of affected individuals.
References
1. Smith, J., & Johnson, L. (2021). "The Role of Testosterone in Sleep Regulation: A Review." *Journal of Sleep Research*, 30(2), 123-130.
2. Brown, A., et al. (2022). "Secondary Hypogonadism and Its Impact on Sleep Quality: A Longitudinal Study." *Sleep Medicine*, 35(4), 456-463.
3. Davis, M., & Wilson, R. (2023). "Hormonal Influences on Sleep Architecture and Disorders." *Endocrinology Today*, 40(1), 78-85.

- Secondary Hypogonadism's Impact on Cardiovascular Health in American Men [Last Updated On: March 14th, 2025] [Originally Added On: March 14th, 2025]
- Stress and Secondary Hypogonadism: Impacts and Management Strategies for American Men [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Genetic Factors in Secondary Hypogonadism: KAL1, FGFR1, GNRHR Mutations and Treatment Implications [Last Updated On: March 17th, 2025] [Originally Added On: March 17th, 2025]
- Secondary Hypogonadism's Impact on Cognitive Function in American Men [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Secondary Hypogonadism in American Men: Building Essential Support Systems [Last Updated On: March 18th, 2025] [Originally Added On: March 18th, 2025]
- Secondary Hypogonadism's Psychological Impact on American Men: A Holistic Treatment Approach [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Secondary Hypogonadism in American Men: Causes, Diagnosis, and Management Strategies [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Secondary Hypogonadism: Impact on Energy and Treatment Strategies in American Males [Last Updated On: March 20th, 2025] [Originally Added On: March 20th, 2025]
- Exercise Strategies for Managing Secondary Hypogonadism in American Males [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism's Impact on Skin Health in American Men: Causes and Management [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism in American Males: Understanding and Managing Hair Loss [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism and Sleep: Impacts and Improvement Strategies for American Men [Last Updated On: March 21st, 2025] [Originally Added On: March 21st, 2025]
- Secondary Hypogonadism: Symptoms, Causes, and Treatment in American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism: Impacts on Body Composition in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism's Impact on Immune System in American Men: A Comprehensive Overview [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Exploring Alternative Therapies for Secondary Hypogonadism in American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism: Causes, Symptoms, and Treatment for American Males [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism: Causes, Symptoms, and Treatment for American Men [Last Updated On: March 22nd, 2025] [Originally Added On: March 22nd, 2025]
- Secondary Hypogonadism: Impacts on Prostate Health and Testosterone Therapy Considerations [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism in American Males: Links to Anemia and Treatment Strategies [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism: Long-Term Effects and Management in American Men [Last Updated On: March 23rd, 2025] [Originally Added On: March 23rd, 2025]
- Secondary Hypogonadism: Understanding Its Impact on Male Libido and Treatment Options [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism and Autoimmune Diseases: Implications for American Men's Health [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism's Impact on Mood Disorders in American Men: Mechanisms and Therapies [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism: Causes, Diagnosis, and Multifaceted Treatment Approaches [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism: Impacts on American Men's Social Life and Well-being [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism's Impact on Bone Density in American Men: Risks and Management [Last Updated On: March 24th, 2025] [Originally Added On: March 24th, 2025]
- Secondary Hypogonadism and Diabetes: Risks and Management for American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism: Integrating Medical and Psychological Care for American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Exercise Boosts Testosterone: Managing Secondary Hypogonadism in American Men [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Sleep Disorders Linked to Secondary Hypogonadism in American Men: Mechanisms and Implications [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Diagnosis, and Management in American Males [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Environmental Factors and Secondary Hypogonadism in American Men: Causes and Prevention [Last Updated On: March 25th, 2025] [Originally Added On: March 25th, 2025]
- Secondary Hypogonadism: Impact on Fat Distribution and Health in American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism's Impact on Kidney Function in American Males: Diagnosis and Management [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Managing Secondary Hypogonadism and Fatigue in American Males: Diagnosis, Treatment, and Support [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Lifestyle Factors and Management of Secondary Hypogonadism in American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Thyroid Function's Role in Secondary Hypogonadism Among American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Understanding Secondary Hypogonadism: Causes, Symptoms, and Treatment Options for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism: Impacts and Management Strategies for American Men [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism's Impact on Muscle Strength in American Men: Diagnosis and Treatment [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism: Causes, Symptoms, and Treatment Options for American Males [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism's Impact on American Men's Physical Performance and Health [Last Updated On: March 26th, 2025] [Originally Added On: March 26th, 2025]
- Secondary Hypogonadism's Emotional Impact and Holistic Management in American Men [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism and Heart Disease: Risks, Symptoms, and Management for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism and Liver Health: Risks and Management for American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Secondary Hypogonadism in American Males: Causes, Diagnosis, and Management Strategies [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Nutrition's Role in Managing Secondary Hypogonadism in American Males [Last Updated On: March 27th, 2025] [Originally Added On: March 27th, 2025]
- Managing Secondary Hypogonadism in American Males: Stress, Strategies, and Support [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Secondary Hypogonadism's Psychological Impact on Men: A Comprehensive Care Approach [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Secondary Hypogonadism's Impact on Cognitive Function in American Men: A Comprehensive Review [Last Updated On: March 29th, 2025] [Originally Added On: March 29th, 2025]
- Secondary Hypogonadism's Impact on Mood in American Men: Mechanisms and Interventions [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Secondary Hypogonadism: Causes, Symptoms, and Hormonal Therapy Management [Last Updated On: March 30th, 2025] [Originally Added On: March 30th, 2025]
- Secondary Hypogonadism: Impact on Energy and Vitality in American Men [Last Updated On: April 1st, 2025] [Originally Added On: April 1st, 2025]
- Managing Secondary Hypogonadism: The Crucial Role of Diet and Nutrition in American Men [Last Updated On: April 4th, 2025] [Originally Added On: April 4th, 2025]
- Secondary Hypogonadism in American Males: Impact on Weight and Management Strategies [Last Updated On: April 5th, 2025] [Originally Added On: April 5th, 2025]
- Sleep's Critical Role in Managing Secondary Hypogonadism in American Males [Last Updated On: April 6th, 2025] [Originally Added On: April 6th, 2025]
- Managing Secondary Hypogonadism: Symptoms, Causes, and Treatment for American Males [Last Updated On: April 7th, 2025] [Originally Added On: April 7th, 2025]
- Managing Secondary Hypogonadism: Holistic Approaches and Increased Awareness in American Males [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Secondary Hypogonadism's Impact on Emotional Resilience in American Men [Last Updated On: April 8th, 2025] [Originally Added On: April 8th, 2025]
- Secondary Hypogonadism: Impact on American Men's Relationships and Coping Strategies [Last Updated On: April 9th, 2025] [Originally Added On: April 9th, 2025]
- Secondary Hypogonadism's Impact on Mental Clarity in American Men: Insights and Treatment [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Managing Secondary Hypogonadism in American Men: Diagnosis, Treatment, and Lifestyle Strategies [Last Updated On: April 10th, 2025] [Originally Added On: April 10th, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Causes, and Management in American Males [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Community Support Enhances Life Quality for Men with Secondary Hypogonadism [Last Updated On: April 11th, 2025] [Originally Added On: April 11th, 2025]
- Secondary Hypogonadism: Impacts on Daily Life and Treatment Options for American Men [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Secondary Hypogonadism in American Males: Impacts on Mental Health and Comprehensive Management [Last Updated On: April 13th, 2025] [Originally Added On: April 13th, 2025]
- Managing Secondary Hypogonadism in American Males: Personalized Approaches and Holistic Care [Last Updated On: April 14th, 2025] [Originally Added On: April 14th, 2025]
- Secondary Hypogonadism: Impacts on Muscle, Bone, Fat, Heart, and Sexual Health in Men [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Understanding Secondary Hypogonadism: Impacts and Management Strategies for Men's Vitality [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Secondary Hypogonadism in American Males: Causes, Diagnosis, and Management Strategies [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Understanding Secondary Hypogonadism: Causes, Symptoms, and Treatment for American Males [Last Updated On: April 15th, 2025] [Originally Added On: April 15th, 2025]
- Understanding Secondary Hypogonadism: Symptoms, Diagnosis, and Management in American Males [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Secondary Hypogonadism: Understanding Its Emotional Impact on American Men [Last Updated On: April 16th, 2025] [Originally Added On: April 16th, 2025]
- Nutrition's Role in Managing Secondary Hypogonadism: Key Nutrients and Dietary Strategies [Last Updated On: April 17th, 2025] [Originally Added On: April 17th, 2025]
- Secondary Hypogonadism: Symptoms, Diagnosis, and Holistic Management for American Males [Last Updated On: April 19th, 2025] [Originally Added On: April 19th, 2025]
- Secondary Hypogonadism in American Males: Lifestyle Factors and Management Strategies [Last Updated On: April 20th, 2025] [Originally Added On: April 20th, 2025]
- Secondary Hypogonadism: Impact on Self-Esteem and Holistic Management Strategies [Last Updated On: April 20th, 2025] [Originally Added On: April 20th, 2025]
- Lifestyle Factors Impacting Secondary Hypogonadism in American Males: A Multicenter Study [Last Updated On: April 22nd, 2025] [Originally Added On: April 22nd, 2025]
- Genetic and Environmental Factors in Secondary Hypogonadism Among American Males [Last Updated On: April 23rd, 2025] [Originally Added On: April 23rd, 2025]
List of USA state clinics - click a flag below for blood testing clinics.
Word Count: 587


















































